
Dr. Michael G. Fehlings, senior scientist at Krembil Brain Institute at Toronto Western Hospital, seen above, believes it’s now more important than ever that people recognize the signs of degenerative cervical myelopathy (DCM).Fred Lum/The Globe and Mail
At Toronto Western Hospital, neurosurgeon Dr. Michael Fehlings frequently encounters patients with degenerative cervical myelopathy (DCM), whose disabilities might have been avoided, if only they had recognized the early signs of their condition.
DCM is the leading cause of spinal cord impairment in adults, which can rob people of their mobility and independence if left untreated. An estimated one in 10 people will eventually develop the condition, which is commonly diagnosed among patients over the age of 50. And as the proportion of older Canadians rises, Fehlings believes it’s now more important than ever that people recognize the signs.
“People need to be aware of this,” says Fehlings, who is also a senior scientist at the Krembil Brain Institute. “It’s an important cause of neurological impairment, and there are effective treatments available now.”
To spread the word among primary care physicians and specialists, Fehlings led a group in creating clinical practice guidelines in 2017, offering new recommendations on how to manage mild, moderate and severe DCM. But still, he often sees patients with DCM, whose symptoms of tingling hands or neck pain were previously misidentified as carpal tunnel syndrome or dismissed as part of normal aging.
Here’s what you need to know about DCM:
What it is:
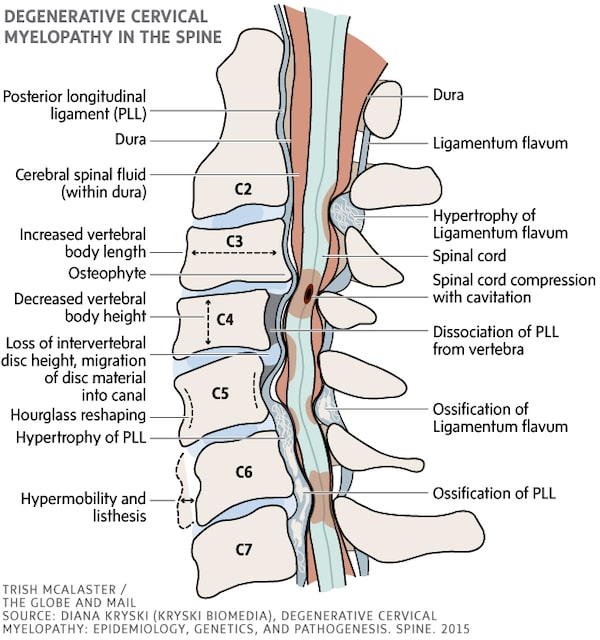
DCM involves compression and injury to the spinal cord, which, over time, can cause serious disability, says Fehlings. This occurs when the discs between vertebrae wear out, leading to bulging of the discs, or when the ligaments around the spine ossify – that is, harden into bone.
An estimated one in 10 people will eventually develop DCM, which is commonly diagnosed among patients over the age of 50.
There is not much people can do to prevent this from happening. One of the main causes, a condition called OPLL (ossification of the posterior longitudinal ligament), is not preventable. The cause of OPLL is unclear, although there are genetic factors and the condition is more prevalent among patients of Asian descent. However, Fehlings says, smoking is a known risk factor for cervical spondylosis, a degenerative disc disease that is another main cause of DCM. Besides abstaining from smoking, he recommends avoiding repetitive trauma, such as extreme weight lifting that puts heavy loads on the neck.
The symptoms:
About 50 per cent of patients who are diagnosed with DCM initially report having neck pain, a symptom that should prompt a look at whether there’s any compression of the spinal cord, Fehlings says.
“In some regards, [neck pain] is a little bit like high blood pressure,” he says. In other words, it can be a red flag of something very serious.
Early on, patients may also experience some impairment in their walking, although they tend to downplay this symptom, shrugging it off as clumsiness. Doctors can recognize this by asking patients to walk in a straight line, heel-to-toe.
“If you’re stumbling all over the place, then that’s a problem,” he says.
Another common symptom is numbness and tingling in the hands. Patients may begin to have subtle difficulties with tasks requiring fine motor control, such as doing up buttons, handwriting or sewing. These symptoms are commonly misdiagnosed as carpal tunnel syndrome, Fehlings says.
A further sign there may be something wrong with the spinal cord is what’s known as “radicular” arm pain, or pain that radiates down the arm.
So, even if people don’t have neck pain, he says, they could have DCM if they experience some of these other symptoms.
The standard diagnostic tool to confirm whether someone has DCM is magnetic resonance imaging (MRI).
The treatment:
Patients with mild symptoms should be monitored and may benefit from physiotherapy, Fehlings says, adding surgery may be offered as an option. But in some cases, if their condition deteriorates, surgery is required.
Other patients may remain stable, but he warns they should nevertheless avoid high-risk activities, since DCM is a common underlying cause of spinal cord injury. Fehlings explains, for example, he recently operated on a patient, who likely had undiagnosed DCM. Because the patient was unstable walking, he fell, injuring his spinal cord, and is now quadriplegic. The take-away? If you know you have DCM, it’s probably best if you avoid mountain-biking or horse-back riding.
Fehlings recommends surgery for those with moderate to severe impairment. Surgery is performed to take pressure off the spinal cord, and in some cases, to reconstruct areas of weaknesses. For instance, this can involve removing the discs, and placing a bone graft into the disc space to open it up, then correcting the alignment of the spinal cord, and reconstructing the area of the spine with a titanium implant.
Most patients only need surgery once, he says, but as they age, some may need further surgery on untreated areas of the spine.
Live your best. We have a daily Life & Arts newsletter, providing you with our latest stories on health, travel, food and culture. Sign up today.
 Wency Leung
Wency Leung