As part of the 150th anniversary of Canada's confederation, The Globe and Mail looks at the Canadians, products and discoveries that changed the world.
When he was admitted to Toronto General Hospital in December, 1921, Leonard Thompson, a 14-year-old with juvenile diabetes, was barely clinging to life. He weighed just 65 pounds and despite a starvation diet of 450 calories a day – the only treatment available at the time – his blood glucose was dangerously high.
On Jan. 22, 1922, Leonard was injected with an experimental treatment called isletin. The impact was negligible.
But, 12 days later, researchers tried again. After the injection, Leonard's blood glucose fell dramatically, to 6.7 millimoles per litre from 28.9 mmol/L. He was discharged from hospital and began to eat more and gain weight.
Within days, six other desperately ill Toronto children received a similar injection, with the same miraculous results. As long as they took an injection daily, their symptoms were largely kept in check.

DONOR PANCREAS
PANCREAS
1
Donor pancreas
A healthy
pancreas
produces insulin
2
Islet harvesting
Insulin- producing
islets, in the
pancreas, are
harvested
3
Islets introduced
Islets are introduced
to the recipient liver
through the portal
vein
RECIPIENT LIVER
(with Type 1 diabetes)
LIVER
4
Insulin from islets
The transplanted islets
secrete insulin in the liver
CARRIE COCKBURN/THE GLOBE AND MAIL,
SOURCE: DIABETES RESEARCH INSTITUTE,
UNIVERSITY OF MIAMI

DONOR PANCREAS
PANCREAS
1
Donor pancreas
A healthy
pancreas
produces insulin
2
Islet harvesting
Insulin- producing
islets, in the
pancreas, are
harvested
3
Islets introduced
Islets are introduced
to the recipient liver
through the portal
vein
RECIPIENT LIVER
(with Type 1 diabetes)
LIVER
4
Insulin from islets
The transplanted islets
secrete insulin in the liver
CARRIE COCKBURN/THE GLOBE AND MAIL,
SOURCE: DIABETES RESEARCH INSTITUTE, UNIVERSITY OF MIAMI
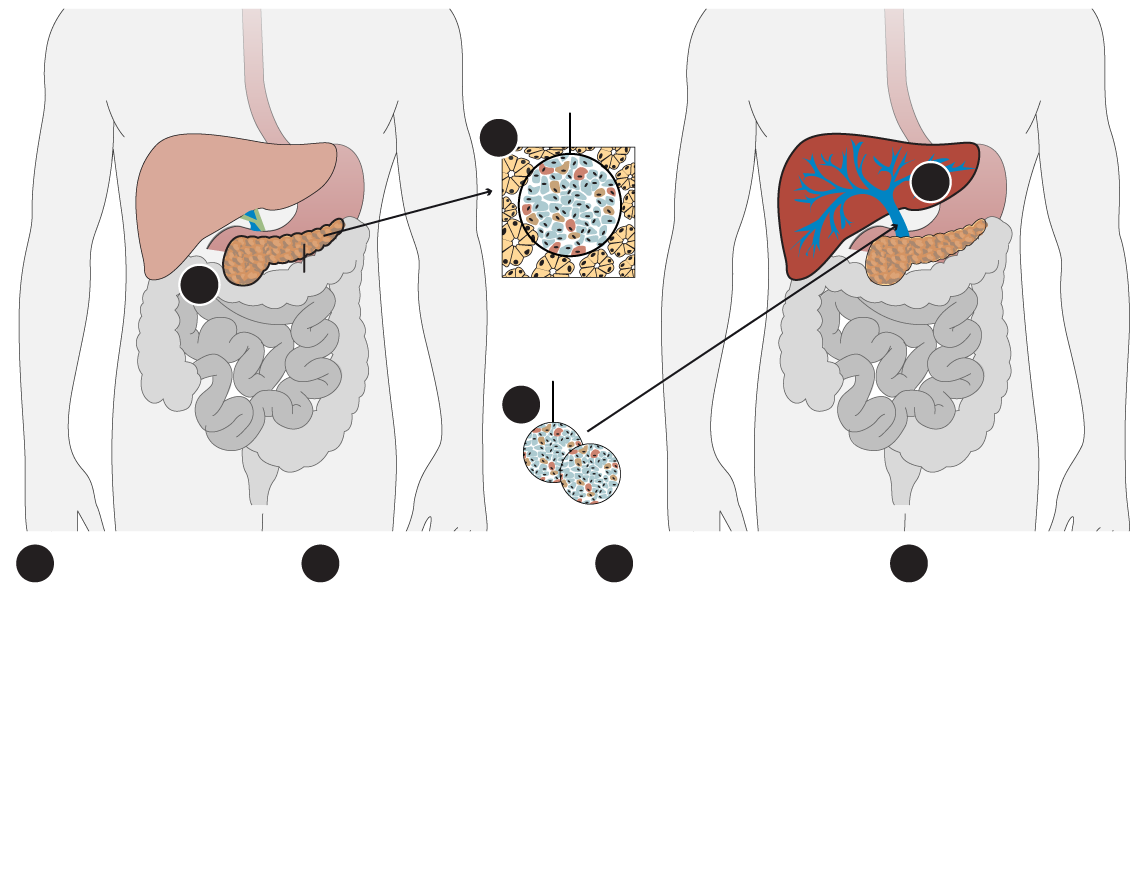
Insulin-producing
islet in the
pancreas
DONOR PANCREAS
RECIPIENT LIVER
(with Type 1 diabetes)
2
LIVER
4
1
PANCREAS
Separated
islets
3
1
2
3
4
Donor pancreas
A healthy
pancreas
produces insulin
Islet harvesting
Insulin- producing
islets, in the
pancreas, are
harvested
Insulin from islets
The transplanted
islets secrete
insulin in the liver
Islets introduced
Islets are
introduced to
the recipient liver
through the portal
vein
CARRIE COCKBURN/THE GLOBE AND MAIL, SOURCE: DIABETES RESEARCH INSTITUTE, UNIVERSITY OF MIAMI
That drug, renamed insulin, forever changed the lives of people with diabetes. It is one of the great medical discoveries of all times, a Canadian innovation that has saved millions of lives.
Before insulin, children with juvenile diabetes (now called Type 1) lived only 1.4 years on average after diagnosis. Adults fared only slightly better: One in five lived 10 years after diagnosis, but with severe complications such as blindness, kidney failure, stroke, heart attack and the necessity to amputate limbs.
Today, people with Type 1 diabetes have an almost normal life expectancy.
"Insulin is the elixir of life for me.
I literally couldn't live without it," says Christine Turner, the director of community engagement at JDRF (formerly the Juvenile Diabetes Research Foundation).
The 46-year-old
Torontonian was diagnosed with Type 1 diabetes at the age of 18 months. She is one of about 300,000 Canadians who live with Type 1 diabetes.
The insulin she takes every day is fundamentally similar to what Dr. Frederick Banting and Dr. Charles Best injected into a dying boy almost a century ago, but there have been many refinements over the years, and in particular since the 1980s.
Today's insulin is no longer derived from the pancreata of cows and pigs, but genetically engineered in the lab and derived from human cells. Instead of one-a-day shots and strict dietary restrictions (to avoid spikes in blood glucose), insulin needs can now be adjusted to food intake.
Insulin is also far easier to administer. Instead of the thick needles and vials of yore, patients today use small, preloaded disposable syringes or pens to inject or, like Ms. Turner, a tiny insulin pump and cannula that delivers the drug when needed.
"Type 1 used to be in the driver's seat, dictating what I could and couldn't do in my life; now Type 1 is in the passenger seat," she says.
That doesn't mean it was always easy. When Ms. Turner was diagnosed as a toddler, she was gravely ill, to the point where she had a blue tinge and she was slipping into a coma when rushed to the hospital.
After the diagnosis, her parents had to pin her down to give her injections and strictly monitor her diet. Then, in the puberty years, she suffered seizures (insulin is a hormone and growth and sex hormones affect insulin resistance) and needed glucagon, an emergency treatment for hypoglycemia, on several occasions.
"It's been scary sometimes but I've been lucky to not have too many health challenges," Ms. Turner says.
The word diabetes, in its original Greek, means "to go through" – so named because the disease drains patients of more fluid than they consume. (Thirst and frequent urination are common symptoms.)
It has also long been associated with sugar. Ancient Hindu texts note that ants were attracted to the urine of people with the mysterious emaciating disease and, for a long time, the illness was diagnosed by having "water tasters" drink urine of patients to test its sweetness. To this day, diabetes is sometimes known colloquially as "the Sugar."
The insulin pump is a device the size of a bar of soap that functions like a pancreas, injecting insulin into the body.
Michelle Siu/The Globe and Mail
For a long time, the treatments used were barbaric and largely ineffective. The Egyptians treated the condition by feeding sufferers earth and ground bones. Then there were the classics, such as bleeding, cupping and blistering. Then, when the importance of blood glucose became clear, there were low-carbohydrate diets and fasting diets, where children literally starved to death. But no treatment was effective until insulin.
There are two principal types of diabetes. In Type 1, the body's immune system destroys the cells that release insulin. In Type 2, which tends to develop later in life, the body can't use insulin properly. Without insulin, cells cannot absorb sugar (glucose), which they need to produce energy.
"Think of insulin as the key that lets sugar into the cells," says Dr. Jan Hux, the chief science officer at Diabetes Canada. "In Type 1, the key is lost; in Type 2, the key is not working very well."
All Type 1 patients need insulin, but only a small percentage of those with Type 2 need injections. The real challenge with insulin, Dr. Hux said, is that it has a very narrow safety range. "You need to constantly juggle because too high and too low can both cause a lot of damage," she said.
People with Type 1 diabetes can suffer from diabetic coma caused by critically low blood sugar, or from ketoacidosis, a buildup of acids in the blood caused by a lack of insulin in the body, both of which can be fatal.
Dr. Banting, a surgeon, became fascinated with the pancreas, an organ known to produce digestive juices and an unknown substance that regulated blood glucose. He believed that if he could shut down production of the digestive juices, he could isolate the other substance.
Along with his assistant Dr. Best, a medical student, he conducted experiments on dogs. When the pancreas was removed, the dog developed diabetes. When the pancreas of a dog was tied up to stop the flow of nourishment, the animal developed digestive problems but not diabetes.
So the researchers took the partly functioning pancreas, ground it up and injected the liquid into the other dog, which alleviated symptoms. The substance they derived from a tiny part of the pancreas was a hormone called insulin.
Dr. Banting and Dr. Best managed to keep the diabetic dog alive for 70 days, and became convinced the treatment would work on humans.
The work was supported by Dr. John Macleod, a diabetes researcher at the University of Toronto. Dr. Bertram Collip, a biochemist, also played a key role, helping the team extract and purify insulin. (They quickly moved from dogs to pigs and cows, whose organs were easier to obtain in large quantities.)
The 1923 Nobel Prize in Physiology or Medicine was awarded to Dr. Banting and Dr. Macleod. Dr. Best and Dr. Collip were not formally recognized. The relationship between the four was often bitter and acrimonious, a story told brilliantly by the late historian Michael Bliss in his book The Discovery of Insulin.
Amazingly, the researchers did not profit financially from their discovery. Rather, they sold the patent to the University of Toronto for $1, saying no one should profit from a lifesaving medication.
To this day, insulin remains a remarkably cheap drug. In Canada, it costs between three and six cents per unit, and a person with Type 1 diabetes would typically use 40 units daily, or about $1.20 worth. (In the U.S., where drug prices are not regulated like Canada, insulin costs have been soaring so that a U.S. patient can pay 10 times as much as a Canadian.) "I've been watching with horror the U.S. experience with insulin," Dr. Hux says.
She noted, however, that insulin itself is just a small part of the cost of treating diabetes. Patients need to regularly test their blood glucose so they have to pay for test strips or glucose meters. Many people with Type 1 diabetes use insulin pumps, which are not always covered by provincial health plans. The same is true of drugs used to stave off heart disease.
"In this country, it's a patchwork quilt. Coverage is all over the map," Dr. Hux says.
A Diabetes Canada survey found that patients spend between $1,900 and $2,600 out-of-pocket. Ms. Turner says she has been lucky to always have private insurance to cover the cost of her medication and supplies, but recognizes that others struggle to pay for their essential medicine.
"Insulin is an elixir, but it shouldn't be an expensive elixir," she says.
Insulin is also a treatment, a life-long treatment, not a cure.
Type 1 diabetes, in many ways, also remains a mystery. The exact cause is unknown. In most people, the body's immune system – which normally fights off harmful bacteria and viruses – mistakenly destroys the insulin-producing cells in the pancreas. Genetics may be to blame, and exposure to certain environmental factors, such as viruses, may trigger the disease.
But, to this day, the scariest aspect of Type 1 diabetes is that it seems to come out of nowhere and sicken children.
"I think the biggest fear for people is the fear of the unknown," Ms. Turner says. "It's a shock at first but I think a lot of us have shown you can live a good life with Type 1 diabetes, and we have insulin to thank."
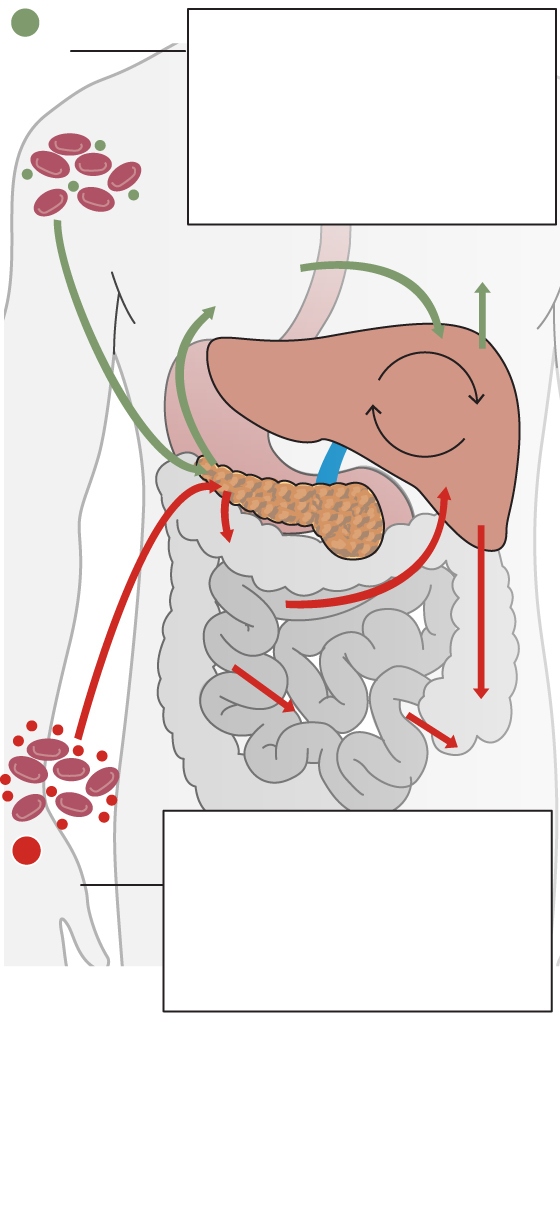
1
People with Type 1 diabetes
have a total lack of insulin.
Without insulin, cells cannot
absorb glucose, which they
need to produce energy. They
can suffer from dangerously
high blood glucose.
HIGH
BLOOD
GLUCOSE
Glucagon released
by alpha cells
of pancreas
Raises
blood sugar
LIVER
glucose*
glycogen*
PANCREAS
Insulin
released by
beta cells
of pancreas
Tissues
take up
glucose
from blood
Lowers
blood
sugar
People with Type 2 diabetes
cannot use insulin effectively.
They tend to have high levels of
blood glucose, which causes
damage to blood vessels and a
host of complications.
2
HIGH
BLOOD
GLUCOSE
*Insulin stimulates the liver to remove glucose from the blood and stores it as glycogen.
Glucagon stimulates the conversion of stored
glycogen in the liver into glucose.
CARRIE COCKBURN/THE GLOBE AND MAIL,
SOURCE: THE SCIENTIST
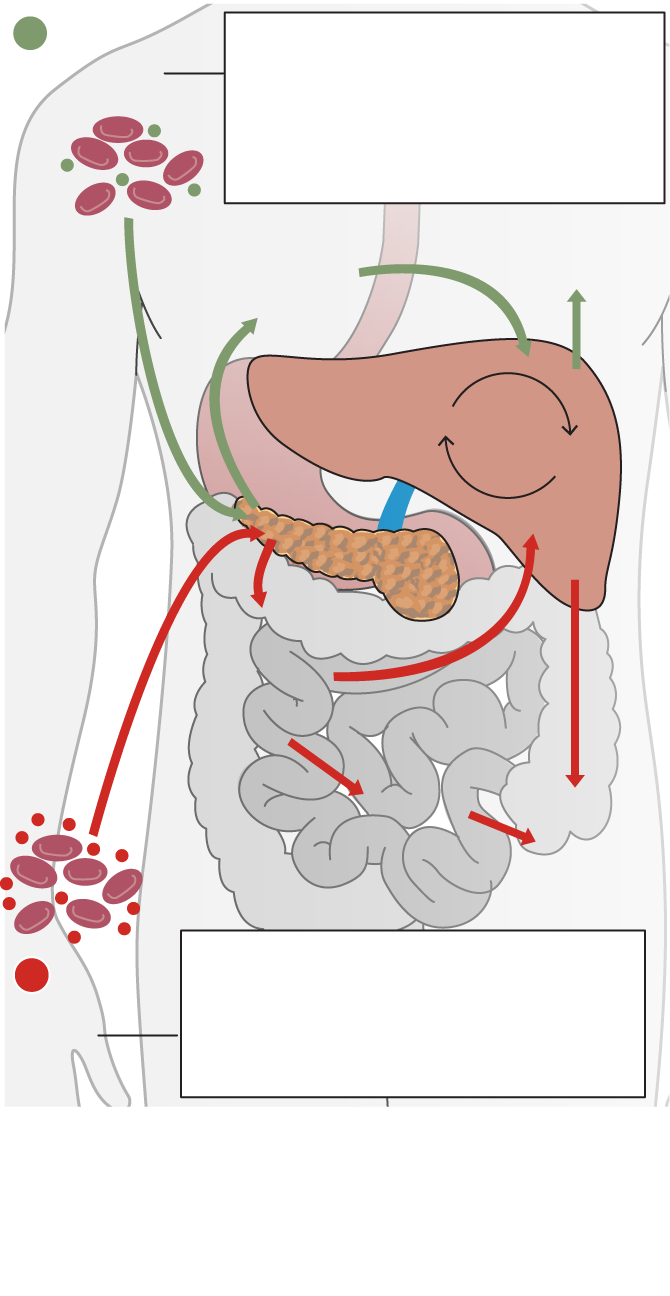
1
People with Type 1 diabetes have a
total lack of insulin. Without insulin,
cells cannot absorb glucose, which
they need to produce energy. They
can suffer from dangerously high
blood glucose.
HIGH BLOOD
GLUCOSE
Raises blood
sugar
Glucagon released
by alpha cells of
pancreas
glucose*
LIVER
glycogen*
PANCREAS
Insulin
released by
beta cells
of pancreas
Tissues
take up
glucose
from blood
Lowers
blood
sugar
People with Type 2 diabetes cannot
use insulin effectively. They tend to
have high levels of blood glucose,
which causes damage to blood vessels
and a host of complications.
2
HIGH
BLOOD
GLUCOSE
*Insulin stimulates the liver to remove glucose from the blood and stores it as glycogen.
Glucagon stimulates the conversion of stored
glycogen in the liver into glucose.
CARRIE COCKBURN/THE GLOBE AND MAIL, SOURCE: THE SCIENTIST

People with Type 1 diabetes have a total lack of
insulin. Without insulin, cells cannot absorb
glucose, which they need to produce energy. They
can suffer from dangerously high blood glucose.
1
HIGH BLOOD GLUCOSE
Raises
blood sugar
Glucagon released
by alpha cells of
pancreas
Insulin
stimulates
the liver to remove
glucose from the blood and stores it as glycogen
LIVER
glucose
glycogen
Glucagon stimulates the conversion of stored
glycogen in the liver into glucose
PANCREAS
Insulin released
by beta cells
of pancreas
Tissues take up
glucose from
blood
Lowers
blood sugar
People with Type 2 diabetes cannot use
insulin effectively. They tend to have high levels
of blood glucose, which causes damage to blood
vessels and a host of complications.
2
HIGH BLOOD GLUCOSE
CARRIE COCKBURN/THE GLOBE AND MAIL, SOURCE: THE SCIENTIST
Researchers make strides in treatment of diabetes
What if, instead of a drug that people with Type 1 diabetes have to inject every day, you could retrain the body to produce its own insulin?
That's exactly what researchers in Edmonton have done in the most promising development in diabetes care since the discovery of insulin in 1922, with a treatment that may cure or dramatically reduce the need for insulin for those with diabetes.
What they do is devilishly simple: Take islets of Langerhans – clusters of cells in the pancreas that produce insulin – and transplant them into patients whose islets have been destroyed by their immune system.
"It's a simple procedure – we poke the patient in the side with a needle, and inject the cells into the liver where they nest and produce insulin," says Dr. James Shapiro, the Canadian research chair in transplant surgery and regenerative medicine at the University of Alberta in Edmonton.
So far, the Edmonton team has done transplants on 261 people, with largely favourable results. (Thousands of islet transplants have been done elsewhere in the world.)
But that's a drop in the bucket considering that there are 300,000 Canadians with Type 1 diabetes. There are two major challenges to scaling up: A dire shortage of organs, and the fact that, like all transplant patients, recipients need to take powerful anti-rejection drugs.
Doing an islet-cell transplant requires cells from at least two pancreata, and the operation often needs to be repeated because effectiveness wanes. (The 261 patients have undergone a total of 591 transplants.)
Jason Turner got his first islet cell transplant in 2005, and has had two more since, the most recent this past April. "It's fabulous. It's changed my life," he says.
Mr. Turner was diagnosed with Type 1 diabetes at the age of 11, and managed well until his 20s. But he had dangerously wild swings in his blood glucose levels and a raft of increasingly severe complications, including digestion problems, diabetic retinopathy (damage to the small blood vessels in the eye that can cause blindness) and neuropathy (pain, tingling and loss of feeling in the limbs that can lead to amputation).
Because of the severity of his symptoms, Mr. Turner was accepted into the research project testing islet-cell transplants. The operation itself was easy, he said; he even remained awake during the procedure.
"I remember looking up at the IV bag with the islet solution in it and thinking: 'This is a really big moment in my life,'" Mr. Turner said of the first time he had the treatment.
The islet cells start working right away and, by the next day, his need for insulin had already decreased by two-thirds – from 45 units to 15. The "crazy highs and lows" in blood sugar stopped, but he continued to need to inject insulin, so a second transplant was performed in 2007. This time the procedure was more successful and Mr. Turner stopped using insulin altogether from 2008-15, something that, until islet-cell transplants succeeded, was unthinkable for someone with Type 1 diabetes.
Then, there was another partial relapse, and he began using low doses of insulin again, until this past Christmas when he saw his blood glucose rise significantly again. A third transplant was done. "And, again, I'm back to taking barely any insulin," Mr. Turner said.
He is quick to add that he has suffered few side effects from his regime of immune-suppression drugs. "Do I consider myself cured? No, not really because I still need treatment."
Dr. Shapiro also refuses to use the c-word. "It's a good treatment. Some people are still doing well 18 years after transplant. But 'cure' is a strong, emotive word that I like to avoid." An islet-cell transplant, he says, "cures diabetes but does not end the need for treatment with anti-rejection drugs."
So what's the solution to that problem?
Dr. Shapiro believes that it is stem cells – undifferentiated cells that can be coaxed into becoming islets cells. "That way you can shield cells from the body's immune system and avoid rejection," he says.
So far, this method has been tested in thousands of mice, but it has yet to be tested in humans. Dr. Shapiro says that, in a perfect world, we will one day be able to transplant islet cells into everyone with diabetes, to have their bodies produce the insulin they need.
"We have good drugs and good equipment like insulin pumps, but it can never provide the level of precision of the human body.
"Ultimately, that's what we want. That would be a cure."
- André Picard